Curriculum Transformation

By Tamara M. Shankel ’88, Senior Associate Dean for Medical Student Education
Loma Linda University School of Medicine (LLUSM) launched its Discovery Curriculum in July 2020. This new curriculum was developed over three years with input from multiple faculty educators, following a literature review and seeking best practices from several other medical schools.
The Discovery Curriculum is based on the concept of the “master adaptive learner,” described by Schumacher et al. in Academic Medicine in 20131 and in an American Medical Association MedEd Innovation Series (2020). A master adaptive learner is able to not only provide expert care for routine problems but is also trained to discover and innovate care for patients in new situations and contexts. Developing adaptive learners emphasizes curiosity, growth mindset, self-motivation, and resilience. Our learners today face a world where health care systems are rapidly changing. We desire to create learners who are able to nimbly adapt as new diseases and new systems are recognized.
The Discovery Curriculum was developed with several goals in mind. First, we strove to increase learning integration—both horizontally within content currently being taught and vertically across all four years of the curriculum. The second was to further emphasize topics important to our mission, including service, lifestyle medicine, and the delivery of whole person care to our patients. Our third focus was to create community and promote the well-being of our students. Fourth, we wanted to give students choices to pursue their interests within each year of our curriculum. Finally, we wanted to continue to graduate outstanding clinicians, with additional skills to help them thrive in an ever-changing world.
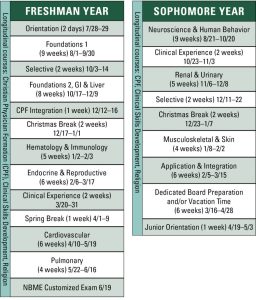
The first 20 months of medical school (see Figure 1) is organized into blocks. Each block integrates multiple basic science disciplines within that system. The first block provides foundational principles necessary for future blocks, and subsequent blocks focus on organ systems. Normal and abnormal physiology and disease processes are integrated throughout the block. Case-based team learning has been expanded in the Discovery Curriculum. Students are given prep material before coming to class, then during class they form teams to work through faculty-developed cases, scenarios, and questions. Thus, they benefit from learning from each other as well as faculty. Quizzes are provided each Friday for students to assess the effectiveness of their learning. These quizzes are discussed by faculty, providing insight into student understanding of concepts and allowing for teaching regarding both content and approach to test questions.
Curiosity and adaptive learning are developed through the patient inquiry curriculum (PIQ), which is the School of Medicine’s unique brand of problems-based-learning that has been championed by schools such as McMasters University and Case Western Reserve. PIQ are student-led case-based sessions where teams of up to 10 students and one faculty facilitator review complex and authentic patient cases. For every case, students: 1. identify learning issues and possible explanations for the patient’s condition; 2. invest time to research textbooks and the primary literature to find answers to their questions; 3. summarize the answers and explanations; 4. present their findings to the team and receive feedback; 5. synthesize mechanistic explanations for patient conditions; 6. develop a differential diagnosis and management plans; and 7. connect and apply relevant health system science, evidence-based medicine, and lifestyle medicine concepts to their patients.
Clinical Skills is a longitudinal course offered throughout the first two years of medical school that focuses on developing history, physical examination, communication, clinical reasoning, and ultrasound skills in students. Students rotate through hospital clinical services for two weeks in year one and year two. Objective standardized clinical exams (OSCEs) during the first two years in the School of Medicine build on well-established OSCE practices but uniquely include a clinical reasoning debriefing component that comes at the end of the patient encounters. During these debriefings, teams of five to seven students work together with facilitation by faculty following a defined clinical reasoning process to develop and defend a differential diagnosis for the patient they just interviewed and examined. These debriefing sessions emphasize the process of cognition and de-emphasize the conclusion of a “right answer.”
Students are given the opportunity to choose unique learning experiences each year of medical school. Selectives in years one and two include varied courses like: Formative Life Narratives; How Medical History and Stories can Change Doctors into Healers; Simulation Skills with Patient Safety; Research Methods; Learning Innovations Lab; Topics on Leadership; Ultrasound; Business of Medicine; Health Systems Science; Lifestyle Medicine; Clinical Informatics and Telehealth; Palliative Care; Patient Safety; Spiritual Care; and Policy, Advocacy, Leadership, and Service, including International Missions, Social Determinants of Health, History of Racism and Medicine, and Immigration and Health.
Certificate tracks in lifestyle medicine, academic medicine, policy advocacy leadership and service, ultrasound, and spiritual care are available for students to use one of their selectives, summer research time, and a fourth-year elective to develop in-depth experience in an area of their choice.
To support the overall well-being of our medical students, we developed LIFE Communities. LIFE Communities are a curricular innovation that provides medical students with a community of peers and faculty mentors for support and connection on their journey to becoming physicians. First-year medical students are assigned to a LIFE Community of 10 students led by a practicing physician mentor. They remain in the same group throughout medical school and meet regularly for mentorship and curriculum. All students now complete a three-year longitudinal course called Christian Physician Formation, the curricular house of LIFE Communities. This class is co-directed by the School of Medicine and the School of Religion and teaches mission-focused topics in the setting of growing relationships. Spiritual formation, community engagement, understanding whole person care and the social determinants of health, building resilience and well-being, understanding one’s professional identity formation, becoming a self-directed lifelong learner, and promoting healthy habits through lifestyle medicine are all components of this curriculum.
Integration weeks are a unique component of the Christian Physician Formation curriculum. First-year medical students spend one week mid-year integrating clinical skills, patient inquiry techniques, and their understanding of the whole person by participating in integrated activities. These activities challenge them to apply compassion, spiritual history skills, and to recognize social determinants of health. For example, each LIFE Community mentor brings their first-year students into the wards during this week to interview a patient from their discipline. Not only do they work on getting the patient’s history, but they also ask, “What matters most to the patient?” including concerns related to food or housing. This experience along with service in their community take students one step closer to understanding the full experience of the patients they will serve.
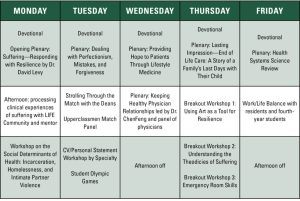
In their third year, students experience two advanced integration weeks. They explore topics that interest them in breakout workshops and discuss in their LIFE Community experiences that were encouraging and challenging from their clinical years. A typical schedule for a student in one of these advanced integration weeks might look like Figure 2. Themes explored during these weeks vary but include delivery of whole person care and God and human suffering.
The third year of medical school begins in May, which is two months earlier than the old curriculum called for, and is organized into two halves. The first half is focused on primary care specialties: family medicine, internal medicine, and pediatrics. The second half encompasses brain health (an integrated neurology and psychiatry rotation), obstetrics and gynecology, and surgery. Each student has two electives in the third year, allowing for dedicated time toward career exploration.
The fourth year of medical school allows for capstone experiences designed to prepare students for residency. Each student completes a sub-internship, an intensive care rotation, an emergency medicine rotation, four weeks of surgery or medicine selectives, and a public health/preventive medicine rotation, which includes a motivational interviewing OSCE and a quality improvement project, in addition to 18 weeks of electives.
The School of Medicine has recently partnered with Kettering Health Network in Dayton, Ohio, and AdventHealth in Orlando, Florida, to develop regional campuses that will continue to provide our students with outstanding opportunities for patient care and clinical education. Students accepted into these tracks will complete their first two years of medical school in Loma Linda and then move to Kettering or Orlando to complete their clinical education.
Outcomes of the Discovery Curriculum, including Step 1, Step 2, performance on the California Consortium for the Assessment of Clinical Competence exam, residency match, and alumni surveys have remained strong and are areas we continue to monitor. Alumni have been integral in the support of our students, providing scholarships, support for students to participate in international missions, and offering housing and support for away rotations. Thank you for your support of our amazing medical students!
Endnotes
- Schumacher, Daniel J. et al. “Developing the master learner: applying learning theory to the learner, the teacher, and the learning environment.” Academic Medicine: Journal of the Association of American Medical Colleges vol. 88, 11 (2013): 1635-45.
 Dr. Shankel is board certified in internal medicine and general pediatrics. She serves as senior associate dean for medical student education for LLUSM.
Dr. Shankel is board certified in internal medicine and general pediatrics. She serves as senior associate dean for medical student education for LLUSM.